When transplant surgeon Dinee Simpson sits in a consultation room with a patient, often they’re joined by the patient’s spouse or children or both.
Sometimes a meeting includes a patient’s cousins or siblings or friends — anyone who will weave together the fabric of support that patient will rely on when he or she receives a new kidney or liver or pancreas.
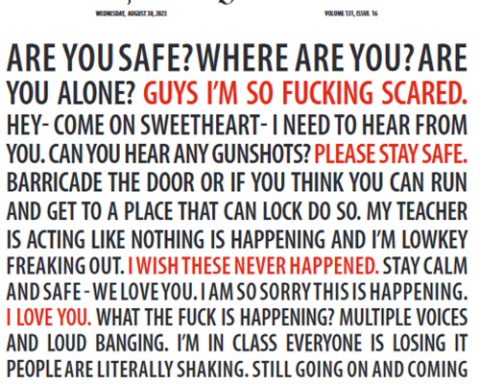
And sometimes, particularly if the patient is black, more than a century of mistrust of the medical community also joins them in the room.
“I’ve had patients tell me that they know transplant is experimental,” Simpson said. “I’ve had patients tell me they know white people get preference when it comes to time on the waiting list.”
(Neither is true.)
“Patients are very frank with me in telling me they know things are unfair or experimental, and they’re the hardest to convince otherwise,” Simpson said. “Those are some of the most heartbreaking cases for me.”
In some families, a deeply ingrained sense of betrayal, passed down through generations, can permeate doctor visits. It’s a product of medical experiments widely performed on slaves in the mid-1800s, a product of the 40-year Tuskegee syphilis experiment, begun in 1932, that denied hundreds of black men a proper diagnosis or treatment for a debilitating disease, a product of quality medical care existing just out of geographic reach.
Simpson understands that in her bones, even as she tries everything in her power to assuage that sense of betrayal and help patients leave it in the past.
Simpson, 40, is Northwestern Memorial Hospital’s first female, African-American transplant surgeon. March marks her one-year anniversary with the hospital. She is the only black, female organ transplant surgeon in Chicago.
“I’m here to serve everybody,” Simpson said, “But there’s a specific population that I feel has a disadvantage, because of social issues, because of genetic predispositions, because of a lot of reasons. They need assistance, and I recognize that I can provide some of that assistance just by looking the way I look.”
After completing medical school at New York University, Simpson moved to Boston for a medical residency through Harvard University.
“I had patients cry,” she said. “I had patients hug me. The reaction was incredible, simply because I looked like them. I was just a trainee. I didn’t have any special medical expertise or background at that point. That’s what sort of sealed my path and pushed me down this road.”
Simpson majored in chemistry at Colgate University and was on track to pursue a career discovering and researching new drugs when, during her junior year, her doctor discovered a suspicious mass in her breast. She had surgery to have it removed.
“It was benign,” she said. “But there was something so profound for me about what that surgeon provided for me. I had fear, I had unknowns. And when I came out of that surgery, I had an answer. I knew the mass was gone. That was really powerful to me.”
She knew, at that point, she wanted to go to medical school. But it was too late to apply for the following year, so she took a job at a tech startup in New York. The company collected data on how consumers looked for health care information online and then provided that data to drug manufacturers to help them target their marketing efforts.
“What I realized is many of the commercials didn’t speak to me, didn’t speak to my family members,” she said. “That’s when I realized that health care really needs to speak to people’s culture.”
The following year, she started medical school.
“That sold me,” she said. “Later that day, we did a kidney evaluation clinic and saw six patients. All six were African-American. That blew me away.”
African-Americans suffer from kidney failure at three times the rate of whites, according to the National Kidney Foundation, and make up 35 percent of all patients receiving dialysis for kidney failure, despite making up around 13 percent of the U.S. population.
Chronic liver disease and cirrhosis are among the leading causes of death in African-Americans between 45 and 64 years old, according to the Centers for Disease Control and Prevention.
Now Simpson works in a city whose population is around 33 percent African-American, and she finds herself engaging in sometimes painful, sometimes transformative conversations.
“This country has a dark history, and it’s remembered,” she said. “The thing I try to help patients remember is: That’s the past, and we’ve come a very long way. I’m not trying to hide anything. I’m not trying to sweep anything under the rug. But I also tell patients what the literature says about their disease and how we can help them.”
Regardless of a patient’s race, the transplant process is shrouded in mystery and misunderstanding.
People worry, Simpson said, that they’ll recover only a fraction of their former lives if they receive a new organ.
“I tell them, ‘What you were doing six months before you started getting sick? We’ll get you back to that,’” she said.
People worry, she said, that they’ll be stuck on a waiting list for years and years.
Liver transplants, she explains, are not based on waiting time. Patients are assigned a Model for End-Stage Liver Disease (MELD) score, a scale ranging from 6 to 40, based on the urgency of the disease. If a patient suffers an infection or trauma — a car accident or a broken bone — that can increase his or her MELD score because a diseased liver can’t help the body heal as quickly as it should.
“You can never say with certainty, ‘You’ll get a liver offer today,’” Simpson said. “But we know from experience, usually a patient with a MELD score of 40 will get an offer very soon.”
Kidney transplants are prioritized by waitlist time, and patients rely on dialysis while they wait for a donor kidney. The average wait time in Chicago is seven years, Simpson said.
“Which is one of the reasons we push for living donations,” she said.
Another topic shrouded in mystery.
“Even though we, as a medical community, have found ways to make the risk very small to donors, people are fearful,” she said. “And most of the time we think about a living donor, we think about a family member. Many of our middle-age and older parents would never want to ask a child to donate a kidney.”
As a mother (her sons are 6 and 9), Simpson said she understands that.
“But what I always tell my patients who voice that fear to me is, at the same time as I’m a mother, I’m also a daughter,” she said. “And I’d be very upset with my parents if they didn’t allow me the opportunity to make that decision for myself to be a donor. I think that’s an important message to get out, and that’s not just to the African-American community. That’s to everybody.”
In 2006, transplant surgeon Juan Carlos Caicedo helped launch the Hispanic Transplant Program at Northwestern, which offers care and information in a culturally sensitive way. Providers speak Spanish. They recognize a family’s hierarchy and make sure consultations and decision-making include all the key players.
“Our vision is to have something that mirrors that for our African-American patients in time,” Simpson said.
Simpson joined the National Kidney Foundation of Illinois’ board of directors. She’s been meeting with people from Gift of Hope, the nonprofit agency that coordinates organ and tissue donation in northern Illinois and northwest Indiana.
“I’m new to Chicago,” she said. “I’m trying to meet different people in the community who have an interest or have already been doing this kind of thing, whose mission is closely aligned with what I want to do.”
Save lives, that is.
“Every paper, every study I’ve read, patients want a physician who will sit down and spend quality time with them and talk at a level they understand and answer their questions,” Simpson said. “But we’re a species where we first judge with our eyes, for better or worse. So when people see someone who looks like them, particularly when they’re in a vulnerable situation, it helps.”
Helps assuage fears. Helps build trust. Helps her patients hear her.
“My goal is to get the message out to the community that we’re here, as a program,” Simpson said. “We’re trying to listen to the specific needs of specific groups, and we’re receptive to their fears and concerns, and we want to help.”
Story by Heidi Stevens
Chicago Tribune (Tribune News Service)